24th February 2025 Early-stage pancreatic cancer detected with 85% accuracy A new blood test able to detect early-stage pancreatic cancer with 85% accuracy has been developed by Oregon Health & Science University (OHSU).
Survival rates for pancreatic cancer – one of the deadliest of all cancers – could soon receive a boost, thanks to a new blood test that enables highly accurate detection of the disease at an earlier stage. Researchers at Oregon Health & Science University developed PAC-MANN (or "protease activity-based assay using a magnetic nanosensor"). This uses a small blood sample to detect changes in protease activity, a key indicator of pancreatic ductal adenocarcinoma, or PDAC, the most common and deadly form of pancreatic cancer. Pancreatic cancer is notorious for going undiagnosed until it has reached an advanced stage, when treatment options are limited. Current tests, such as carbohydrate antigen 19-9, are good for indicating prognosis, but lack the sensitivity needed for early-stage detection. "The problem with pancreatic cancer is that we often catch it too late," said Jared Fischer, PhD, a postdoctoral fellow at OHSU who specialises in molecular and medical genetics. "Our goal with PAC-MANN is to give clinicians a tool that can detect the disease much earlier, when more treatment options are available and there is a better chance of survival."
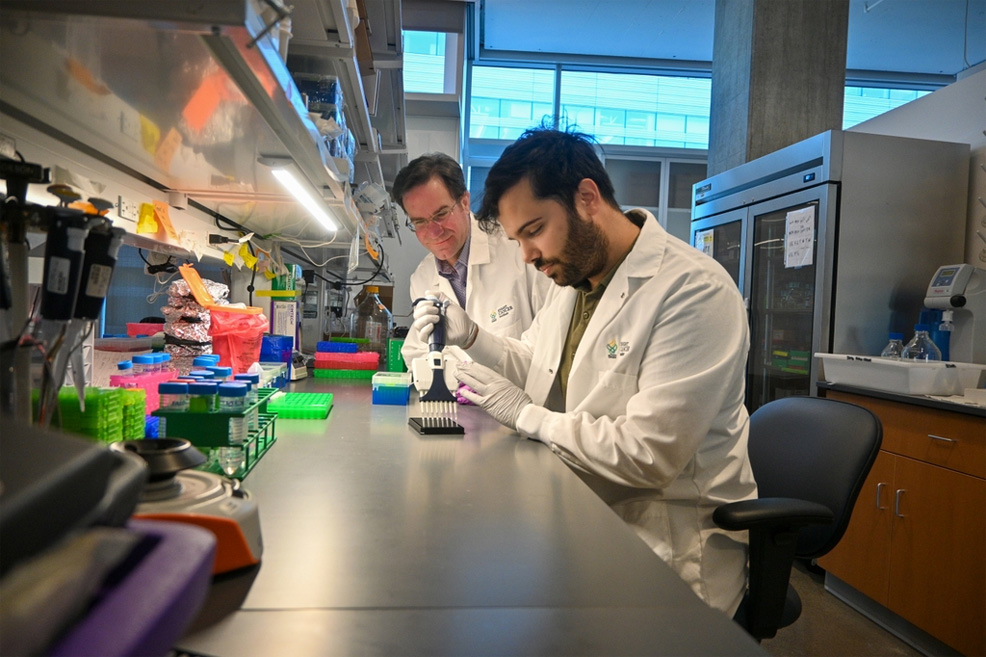
A study describing PAC-MANN is published in Science Translational Medicine. The lead author is Jose Montoya Mira, PhD, also from OHSU, who contributed his extensive knowledge of engineering and biology. This collaboration, which included more than a dozen other scientists, aimed to create a more cost-effective, high-throughput test that could be used anywhere, not just at specialty labs or large medical universities. "Our test could be used for people at high risk of pancreatic cancer, which is not targeted by current tests," explained Dr. Mira. "It allows for a more robust and less invasive screening, unlike an endoscopic ultrasound and other liquid biopsy tests that require large volumes of blood, thus allowing our test to be performed more frequently for earlier detection." The researchers obtained blood samples from 350 patients at the OHSU. These patients either had pancreatic cancer, faced a high risk of developing it, or served as controls. The research team analysed the blood for specific proteins, particularly proteases, which become more active in people with PDAC. By identifying these proteins, they developed a test capable of specifically detecting pancreatic cancer. PAC-MANN correctly distinguished patients with pancreatic cancer from healthy individuals and those with non-cancerous pancreatic issues 98% of the time. Combined with CA 19-9 (the conventional test), it also identified early-stage cancer with 85% accuracy. In addition, the findings showed that PAC-MANN effectively tracked treatment progress. After surgery, researchers observed a decrease in protease activity, indicating that the test may help determine whether treatments are working. "This test isn't just about detection – it could also help us measure how well treatments are working, and guide therapeutic options," said Fischer. "If we can track a patient's response to therapy in real time, we can make better treatment decisions and improve outcomes." Furthermore – unlike traditional tests – PAC-MANN requires only a tiny blood sample and provides a simple fluorescent readout, making it a quick and accessible screening option. "The big difference with this test is the cost. It takes only 8 microlitres of blood and 45 minutes to run at less than a penny per sample," said Montoya. "This could easily be used in rural and underserved settings, where traditional tests are unavailable or impractical." If further validated in clinical trials, PAC-MANN could become a valuable tool for catching pancreatic cancer sooner, giving patients more treatment options and a better chance at survival. For decades, the 5-year survival rate has remained stubbornly low, improving only modestly from 2% in the 1970s to around 13% now. At that pace, reaching a 100% survival rate might seem like a goal for the next century; yet breakthroughs such as PAC-MANN give hope that with innovative detection and treatment strategies, far greater progress could be made in a much shorter time frame. "Hopefully," added Fischer, "this is one step toward ending cancer as we know it."
Comments »
If you enjoyed this article, please consider sharing it:
|
||||||